Recognizing the need for new solutions, the OHA and its Board of Directors began implementing a renewed approach to its advocacy strategy. This long-term approach aims to prepare Ontario's health system for the needs of a growing and aging population, encouraging hospitals to explore innovative technologies and new models of care.
While supporting hospitals with present-day challenges through advocacy and core member services, the OHA continues to encourage hospitals to drive necessary systemic changes. This dual focus on immediate support and future-oriented transformation underscores the OHA's commitment to ensuring a robust and responsive health care system for all Ontarians.
Ensuring Financial and Operational Stability – Keeping Hospitals Whole
Provincial Advocacy
The OHA actively engaged government to address financial pressures facing the hospital sector in 2024-25. Concerned about maintaining access to services, the OHA requested in its Pre-Budget Submission that hospitals be kept financially whole, outlining three key areas of financial pressure: labour costs, non-labour inflation, and service growth. To support their recommendations, the OHA developed and shared resources with members and held an advocacy guidance session providing advice on local advocacy.
The OHA's advocacy efforts involved engagement with various government officials, including the Ministers of Health and Finance, the President of the Treasury Board, and key political staff. Member hospitals also played a crucial role in amplifying the OHA's message through discussions with their local Members of Provincial Parliament (MPPs).
The Temporary Locum Program (TLP) has been a critical tool for ensuring sufficient physician coverage in small, rural, and northern emergency departments. In March 2024, following ongoing advocacy, the province extended the program until March 31, 2025. Looking ahead, the OHA has learned that they will not be extending TLP. However, the government has committed to a permanent solution in TLP's place, which they plan to share in the spring of 2025.
 In March 2024, the Provincial Budget was tabled, allocating a four per cent increase ($965 million) in base funding for hospitals. Additional health sector investments included $743 million to address health human resource challenges, $546 million over three years for primary care teams, and a $50 billion investment in health infrastructure over the next decade.
In March 2024, the Provincial Budget was tabled, allocating a four per cent increase ($965 million) in base funding for hospitals. Additional health sector investments included $743 million to address health human resource challenges, $546 million over three years for primary care teams, and a $50 billion investment in health infrastructure over the next decade.
Following the budget release, the government confirmed its commitment to provide base funding increases for 2024-25 to account for increased compensation costs, although this was not explicitly outlined in the Ontario Budget. The OHA's ongoing advocacy resulted in two tranches of funding being allocated for 2024-25.
In August 2024, the OHA began planning for the 2025-26 provincial Budget, finalizing its recommendations in late 2024. These recommendations address continued in-year financial pressures and aim to ensure appropriate resource allocation for the upcoming budget year.
More recently, in December 2024, the province provided significant additional in-year investments towards hospital base funding of approximately $850 million and targeted in-year pressure funding of $250 million – which came as a direct result of close collaboration and advocacy from the sector to ensure operational stability for 2024/25.
Provincial Health System Planning
The OHA continued its close collaboration with the Ministry of Health (Ministry) and Ontario Health (OH) through the Hospitals Advisory Committee (HAC). The HAC met throughout the year to address pressing financial challenges such as Bill 124, cash flow issues, deficits, capital funding shortfalls, and agency nursing costs. Following the release of OH's Hospital Benchmarking tool in September, the OHA collected feedback from hospital members and conducted a detailed review of the tool's indicators and data quality. These efforts are part of ongoing advocacy to develop high-value tools that minimize the data burden on hospitals.
To address financial challenges in long-term care (LTC), the OHA established the Hospital-Operated Long-Term Care Homes Consultation Group at the request of its members. This group provides guidance on bridging the gap between funding and operating expenses for LTC beds. Financial data collected from 30 hospitals operating LTC beds will inform the OHA's advocacy efforts aimed at securing better support for these facilities. This initiative highlights the OHA's commitment to addressing critical funding gaps in hospital-operated LTC services.
 Under the direction of the OHA's Rehab and Complex Continuing Care (Rehab-CCC) Network, and with support of a sub-committee, the OHA developed a position paper to support Rehab-CCC hospitals in articulating their unique value in the context of current and emerging challenges and identifying opportunities for the sector over the next decade. The content of the document will be used in policy and advocacy materials and in supporting the sector at system planning tables.
Under the direction of the OHA's Rehab and Complex Continuing Care (Rehab-CCC) Network, and with support of a sub-committee, the OHA developed a position paper to support Rehab-CCC hospitals in articulating their unique value in the context of current and emerging challenges and identifying opportunities for the sector over the next decade. The content of the document will be used in policy and advocacy materials and in supporting the sector at system planning tables.
Recognizing the importance of a strong primary care system to hospitals and overall health care delivery, the OHA has been actively collaborating with primary care partners to reduce administrative burdens. The association participates in OH and OntarioMD-led initiatives focused on improving administrative efficiency and supports hospitals in adopting new standards, such as standardized specialist forms. The Physician Leadership Committee (PLC) plays a key role in providing early feedback to ensure smooth implementation of these standards. Additionally, regular engagement with partners like the Ontario College of Family Physicians supports the development of joint strategies for addressing targeted issues within primary care.
The OHA also continues to advocate for incentive models that align with the dual roles of primary care physicians in small, rural, and northern communities who provide both primary and hospital care, including emergency services. Outside of Physician Services Agreement (PSA) negotiations, the OHA assists hospitals in resolving physician remuneration issues related to locum programs, rural and northern agreements, alternative payment plans, and other compensation challenges that affect hospital services. These initiatives underscore the OHA's commitment to supporting hospitals and ensuring equitable physician compensation across Ontario's health system.
Federal Election Preparedness
Over the past year, the OHA has been working to strengthen its relationship with the Government of Canada for the purpose of building a coalition of decision-makers and influencers who can assist the OHA in achieving its policy objectives. Management and staff met with key officials within the Office of the Minister of Health Canada (HC); Department of Innovation, Science and Economic Development (ISED); as well as other influential Members of Parliament, including members of the House of Commons Standing Committee on Health (HESA) and the House of Commons Standing Committee on Science and Research (SRSR).
The aim of these introductory meetings has been to introduce the organization to federal decision-makers and establish a relationship for credible future discussions on issues related to research, health care, mental health, and Indigenous health care. The OHA has also been focusing its outreach on Members of Parliament from the Conservative Party of Canada (CPC), in consideration of the upcoming federal election. Thus far, polls are indicating a strong lead for the CPC.
Federal Pre-Budget Advocacy
The Canadian research landscape is undergoing significant changes, as evidenced by the 2024 Federal Budget tabled in April. This budget included substantial investments in research, a result of extensive advocacy efforts by the OHA, individual hospitals, and system partners. The OHA's pre-budget submission had a singular focus: recommending that the Government of Canada increase its investments in the federal granting councils (Tri-Agency) by at least 10 per cent annually for five years, totalling $2.32 billion.
In addition to increased funding, the government announced new measures to modernize the federal research support system. The goal is to bring strategic vision and enhanced coordination while preserving the elements that have contributed to Canada's strong record of research excellence. A key component of this modernization is the creation of a new capstone research funding organization. Under this new structure, the granting councils will continue to exist, maintaining their focus on supporting excellence in investigator-driven research while actively contributing to the collective and strategic direction of the new organization.
 In response to these developments, the OHA has been proactive in shaping the future of research in Canada. On July 17, 2024, following consultation with its Research and Innovation Committee, the OHA submitted recommendations to the Canada Research Coordinating Committee Secretariat regarding the creation of the new federal capstone research funding organization. To further discuss these recommendations, the OHA met with Dr. Tammy Clifford, President of the Canadian Institutes of Health Research, and her colleagues. In September 2024, the Standing Committee on Science and Research opened an investigation into the Canada Research Coordinating Committee's consultation process and the OHA submitted their willingness to testify on the process and submitted a written brief to reiterate the recommendations, with a focus on those not addressed in the Tri-agency report on the consultation feedback.
In response to these developments, the OHA has been proactive in shaping the future of research in Canada. On July 17, 2024, following consultation with its Research and Innovation Committee, the OHA submitted recommendations to the Canada Research Coordinating Committee Secretariat regarding the creation of the new federal capstone research funding organization. To further discuss these recommendations, the OHA met with Dr. Tammy Clifford, President of the Canadian Institutes of Health Research, and her colleagues. In September 2024, the Standing Committee on Science and Research opened an investigation into the Canada Research Coordinating Committee's consultation process and the OHA submitted their willingness to testify on the process and submitted a written brief to reiterate the recommendations, with a focus on those not addressed in the Tri-agency report on the consultation feedback.
Looking ahead to the 2025/26 Budget, the OHA submitted recommendations to the House of Commons Standing Committee on Finance in August 2024. In anticipation of the provincial election, these proposals were expected to influence the election platforms of major political parties for the 2025 elections, given their broad appeal. The OHA's recommendations included strategies to enhance the commercialization of health research, with a focus on driving innovation and ensuring that research discoveries translate into tangible health solutions and economic growth. This forward-thinking approach demonstrates the OHA's commitment to advancing both health care and economic development through research and innovation.
2025 Update
While these Budgetary announcements were welcomed news, in early January 2025, the Parliamentary session was ended by prorogation, disrupting the introduction and passage of key pieces of legislation. On January 6, Prime Minister Justin Trudeau announced that he would resign as Party Leader and Prime Minister as soon as a new Liberal Leader is selected. Governor General Mary Simon agreed to prorogue Parliament until March 24, providing a short period for the Liberal Party to hold a leadership contest.
As such, any legislation that was intended to be tabled, including the second Budget Implementation Act, will not have an opportunity to be introduced. The health research investments announced in the 2024 Budget, including $1.8 billion over five years for SSHRC, NSERC and CIHR, were intended to be included in the second Budget Implementation Act. These Acts enact the contents of the Budget and are typically priority pieces of legislation. The second Act was not tabled in the fall because of the Opposition filibustering, which effectively stalled any movement of legislation outside of committees in the House of Commons. As such, management is now focused on reinforcing the importance of continued investment in health research in the months ahead.
New and Ongoing Advocacy
In 2024, the OHA actively engaged in various advocacy efforts addressing legal and regulatory developments impacting Ontario hospitals. The OHA continued its work on the legal framework for integrated community health services centres (ICHSC), expressing concerns about location-based restrictions and emphasizing the need for coordinated human resource management, appropriate hospital funding, and comprehensive accountability processes. Additionally, the association advocated for members regarding Bill 194, Strengthening Cyber Security and Building Trust in the Public Sector Act, 2024, which aimed to create new cyber security, artificial intelligence (AI) and privacy-related obligations for hospitals.
Advocacy efforts extended to several other crucial areas within the health care sector. The OHA made submissions on behalf of its members concerning Ontario Health Team (OHT) designation, pharmacy scope of practice, and medical assistance in dying (MAID). The association also facilitated direct member advocacy to the government regarding proposed amendments to the provincial Electronic Health Record under the Personal Health Information Protection Act, 2004 (PHIPA). These wide-ranging advocacy initiatives demonstrate the OHA's commitment to addressing the diverse challenges and opportunities facing Ontario's health system.
The OHA prepared recommendations for the members of the Uninsured Patients Time-limited Advisory Group to use for their advocacy efforts. The document synthesized the issues that arise resulting from a lack of funding to cover hospital and community-based health services for uninsured patients and the advisory group's key recommendations, including the introduction of a permanent and targeted uninsured program. The document was also shared with the Deputy Minister.
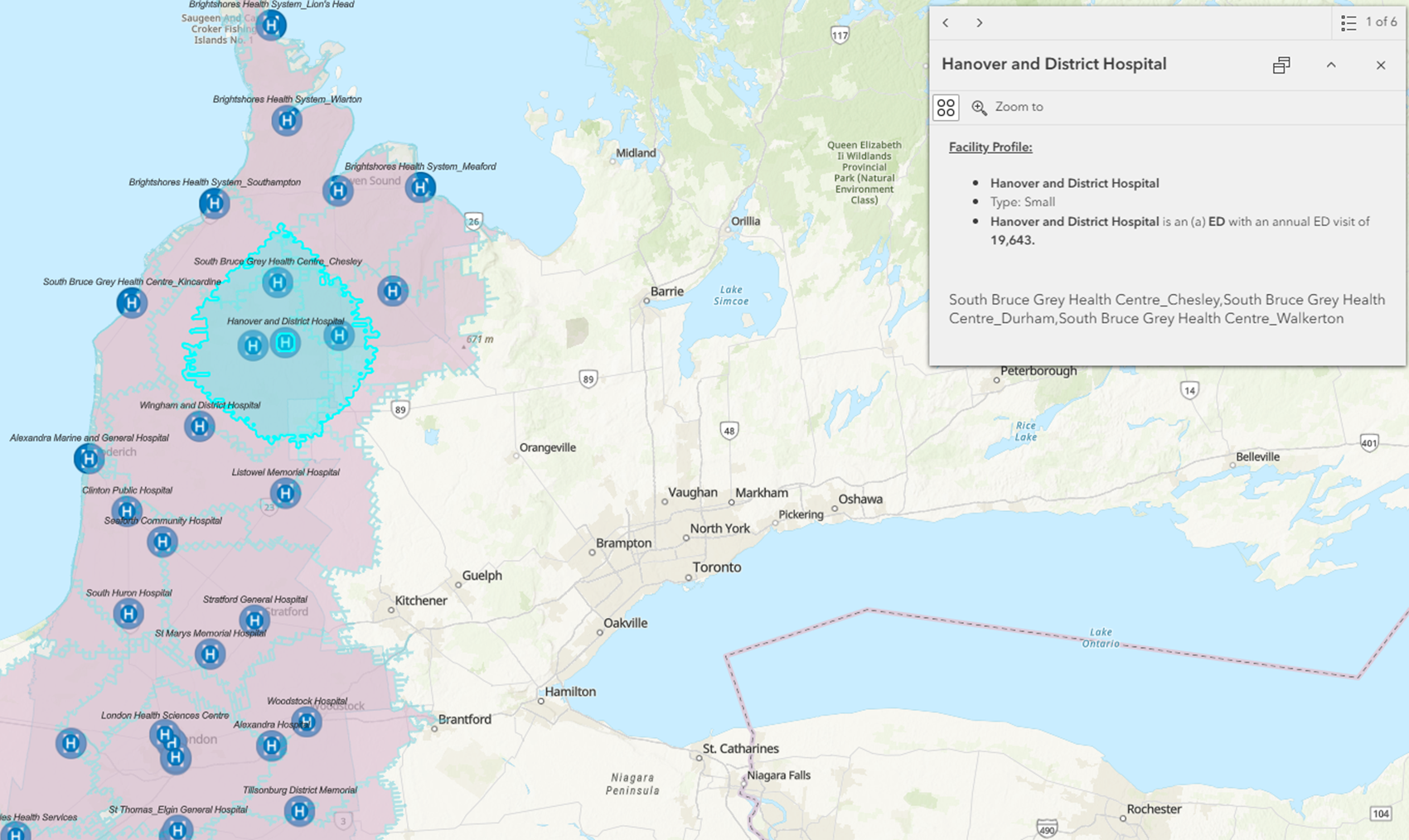 OHA management continues working through the action plan developed in conjunction with the Small, Rural and Northern (SRN) Emergency Department Strategy Advisory Group. As part of this work and to support capacity planning for hospitals in the South-West region, the OHA has been building an interactive map for the South-West Emergency Services Spectrum (SWESS) Committee that details the region's emergency health services and its users (e.g., hospital capacity, volume and wait time data, patient acuity metrics, diagnostic imaging availability). Building the interactive map has been possible as almost all SWESS hospitals leverage the OHA's Information Decision Support platform.
OHA management continues working through the action plan developed in conjunction with the Small, Rural and Northern (SRN) Emergency Department Strategy Advisory Group. As part of this work and to support capacity planning for hospitals in the South-West region, the OHA has been building an interactive map for the South-West Emergency Services Spectrum (SWESS) Committee that details the region's emergency health services and its users (e.g., hospital capacity, volume and wait time data, patient acuity metrics, diagnostic imaging availability). Building the interactive map has been possible as almost all SWESS hospitals leverage the OHA's Information Decision Support platform.
An interactive map was developed to highlight details for the south west region's emergency health services and its users.
The OHA is also continuing its work to support the SRN Emergency Department Strategy Advisory Group in the areas of capacity planning, health human resources (HHR), and intersectoral integration.
Supporting members through engagement, resources and education remains a priority of the OHA's ongoing advocacy efforts. Key initiatives from last year included expanding its Education Committee to include large community hospitals, recognizing their growing role as primary clinical partners for new and expanded medical programs. To support these hospitals in their advocacy efforts for additional financial support, the OHA has provided key messages and plans to establish a working group to ensure alignment among affected institutions.
The OHA has been advocating for a common nursing placement platform to be mandated and funded in all hospitals. In the absence of a common platform, between May and August 2024, the OHA conducted a nursing placement capacity survey to collect information on placements happening in hospitals. The OHA continues to push for a common placement platform.
Evidence-Based Insights
Supporting advocacy efforts from an evidence-based position, the OHA launched foundational pieces of work in 2024. In an updated version of the Ontario Hospitals - Leaders in Efficiency report, the OHA reaffirmed that Ontario's hospitals continue to lead the country in efficiency, despite the increasing pressures of financial instability, HHR challenges, and a rapidly growing and aging population. This report underscores the resilience and adaptability of the hospital sector in the face of ongoing challenges.
Looking towards the future, the Projected Patterns of Illness in Ontario study the OHA commissioned through the Dalla Lana School of Public Health at the University of Toronto, revealed significant strain on the health care system over the next two decades. The data emphasizes the critical need for capacity planning and strategic investments in innovation to ensure adequate support for health services. In response, the OHA has already begun engaging with members and stakeholders to discuss next steps and share this crucial information.
To further understand the financial landscape of Ontario hospitals, the OHA commissioned Deloitte to analyze the working fund position of hospitals over the past six years. The resulting report validated that working capital positions are influenced by operational funding and highlighted the need to address longer-term operational funding in light of pressures such as inflation, aging infrastructure, and growing service demands. These findings will play a crucial role in the OHA's financial advocacy efforts throughout 2025.
The OHA conducted a survey to collect diagnostic and surgical capacity information for MRI, CT, cataracts, as well as hip and knee-replacement procedures. This survey also captured barriers to realizing full capacity. Results showed that Medium-Sized Hospitals are outperforming base volumes for MRI, CT and hip and knee-replacements. The survey results will be used for advocacy with the Ministry for continued support on capacity building in Medium-Sized hospitals.
Harnessing Hospital Leadership and Innovation
Sharing Perspectives: Ontario Hospitals as Leaders in Innovation
 The OHA's renewed advocacy strategy aims to address the population health challenges facing Ontario over the next two decades, emphasizing a focus on determinants of health, prevention, and building capacity across the health care system through innovation and technology, including AI.
The OHA's renewed advocacy strategy aims to address the population health challenges facing Ontario over the next two decades, emphasizing a focus on determinants of health, prevention, and building capacity across the health care system through innovation and technology, including AI.
The OHA communicated this renewed approach through its Health System News (HSN) website, highlighting themes such as hospital-enabled research, innovative solutions for surge demand in care, and showcasing advancements in digital health, virtual care, and AI in health care. Additionally, the OHA's President and CEO Anthony Dale shared an article in the Globe and Mail in September, outlining various aspects of this new strategy and the projected challenges facing Ontario's health system.
Part of the OHA's Innovation Adoption Strategy included interviews with 40 hospital members using or planning to use AI within six months. The collected information provided insights on AI technologies, applications, outcomes, challenges, and integration goals within the hospitals.
A Renewed Focus on Governance
Last year, several initiatives were launched to strengthen hospital governance. A key development was the establishment of the Advisory Committee on Hospital Governance, which held its inaugural meeting in October. The committee plays a vital role in supporting the OHA's efforts related to hospital leadership and governance, guiding advocacy initiatives for recruiting and retaining hospital leaders, and identifying opportunities to enhance governance-related programs and resources. It also provides valuable input on ongoing and emerging governance issues, reviewing and offering feedback on materials and submissions developed by the OHA.
 Additionally, the OHA in collaboration with Borden Ladner Gervais LLP (BLG) ran the Hospital Governance Essentials for New Directors program. This four-part virtual series aimed to familiarize new hospital governors with the legal, governance, and funding frameworks necessary for effective governance in the Ontario hospital sector. Additionally, the Governance Community of Practice continued to serve as a platform for over 130 governance professionals to share resources and collaborate.
Additionally, the OHA in collaboration with Borden Ladner Gervais LLP (BLG) ran the Hospital Governance Essentials for New Directors program. This four-part virtual series aimed to familiarize new hospital governors with the legal, governance, and funding frameworks necessary for effective governance in the Ontario hospital sector. Additionally, the Governance Community of Practice continued to serve as a platform for over 130 governance professionals to share resources and collaborate.
Recognizing the crucial role of hospital board chairs in hospital governance, the OHA introduced a communication called the Board Chair Brief in June. This new initiative aims to keep board chairs well-informed and engaged with current developments, challenges, and opportunities facing Ontario's hospitals.
Growing and Strengthening Core Services
Member Relations, Member Engagement and Knowledge Transfer
Significant progress was made in the second year of the OHA's 2023-2027 Strategic Plan, Advocacy and strategic priorities took shape through focused efforts on critical issues and increased engagement with hospital leaders and boards. As part of this engagement strategy, the OHA actively connected with hospital leadership and boards across the membership, gaining valuable insights into unique regional challenges and providing a platform for direct feedback that informs future advocacy efforts and strategic directions.
The success of these initiatives is reflected in the annual OHA Member Satisfaction Survey conducted in April-May 2024, which revealed a high overall satisfaction rate of 93 per cent with OHA's performance. This marks the tenth consecutive year of over 90 per cent satisfaction, demonstrating the association's consistent commitment to addressing the needs and concerns of its members. The survey, which assesses overall satisfaction, performance in four key areas, and top issues facing hospitals, serves as a crucial tool for the OHA to continually refine its approach and ensure alignment with member priorities.
 In spring 2024, the OHA hosted its flagship event, the Health Care Leadership Summit, which brought together Ontario hospital board chairs and CEOs. The summit focused on reconsidering traditional approaches to health services, examining hospital CEO leadership competencies in a changing environment, and identifying concrete solutions for leveraging AI, technology, innovation, and the health research ecosystem to enhance the adaptability of health care in Ontario. A summary of the event is available for those who were unable to attend.
In spring 2024, the OHA hosted its flagship event, the Health Care Leadership Summit, which brought together Ontario hospital board chairs and CEOs. The summit focused on reconsidering traditional approaches to health services, examining hospital CEO leadership competencies in a changing environment, and identifying concrete solutions for leveraging AI, technology, innovation, and the health research ecosystem to enhance the adaptability of health care in Ontario. A summary of the event is available for those who were unable to attend.
Former Ontario Minister of Health, the Hon. Sylvia Jones addresses attendees of the 2024 Health Care Leadership Summit.
Throughout last year, the OHA collaborated with Borden Ladner Gervais (BLG) and the Healthcare Insurance Reciprocal of Canada (HIROC) to host sessions on various topics. These sessions covered amendments to the Ontario Not-for-Profit Corporations Act, 2010 (ONCA), the newly enacted Fighting Against Forced Labour and Child Labour in Supply Chains Act (Bill S-211), privacy and cyber security considerations stemming from recent Information and Privacy Commissioner decisions, Bill C-295, An Act to amend the Criminal Code (regarding neglect of vulnerable adults), and a recent coroner's inquest (Ryan Inquest).
In 2024, the OHA also introduced the Comms Check virtual series, designed for hospital communicators to share insights and information, encourage dialogue, and facilitate the spread of best practices. Three sessions were held in 2024, focusing on the OHA's renewed advocacy approach, the use of AI to optimize communications and strategies for addressing misinformation in health care. These initiatives demonstrate the OHA's commitment to providing relevant learning and engagement opportunities for members, addressing current challenges in the health care sector, and promoting knowledge sharing among health care professionals.
Expanding engagement to hospitals not previously represented in OHA networks, communities or councils, the association formed a new network for CEOs of large community hospitals. The Network is co-led by Altaf Stationwala (President and CEO, Mackenzie Health) and Lynn Mikula (President and CEO, Peterborough Regional Health Centre). The goal of the network is to provide high-value engagement that keeps members well-informed and balances flow of information between the Network, OHA members, system stakeholders, and government and its relevant ministries.
Management resumed hospital board visits and presentations and has evolved presentation materials to reflect broader conversations on the important role of hospital boards in shaping the future of our health care system. This updated presentation includes a preview of the historical evolution of hospital governance, the legislative landscape, current pressures facing the sector, and the OHA's advocacy efforts. The OHA connected with more than 40 hospital boards over the course of the year. Management anticipates these presentations will continue into the spring and include requests to speak at board meeting portions of hospital annual general meetings in June and July.
New and Updated Member Resources
Continued efforts to keep members informed about the evolving legislative landscape included providing semi-annual legislative and regulatory summaries, covering Fall/Winter and Spring/Summer 2024 updates. These comprehensive summaries offer insights into OHA submissions, resources, recent changes, and potential developments under monitoring.
In March, the OHA released the fifth edition of Understanding Your Legal Accountabilities – A Guide for Ontario Hospitals, to assist health care providers in comprehending their legal responsibilities. Additionally, the organization updated its Hospital Prototype Corporate By-law to align with recent amendments to Ontario's Not-for-Profit Corporations Act (ONCA), which took effect in October 2024, and conducted an information session to support this transition.
Hospital Analytics
Last year, the OHA implemented three key projects to support hospitals with innovative solutions and tools. The enhanced HR Benchmarking Dashboard, launched in the spring, provided hospitals with comprehensive trend data and visualizations to identify improvement opportunities and compare performance across various categories. Responding to member interest, the OHA hosted four Ontario Healthcare Reporting Standards (OHRS) practical application workshops aimed at helping health finance analysts leverage OHRS data for decision-making and information requests. Additionally, in April, the OHA introduced the Local Registration Authority (LRA) portal, an online automated system designed to streamline access control for OHA's data and analytics tools, allowing independent management of access request authorizations and user permissions.
Integrated Decision Support (IDS) is Ontario's most widely used collaborative solution for integrating health services utilization data across providers, with growing interest and expanding coverage. The platform now offers a comprehensive regional view of Ontario Health Toronto-based hospital activity and has integrated data from home and community care support services organizations, creating a province-wide linked data set. IDS has also introduced new data sources, including long-term care and community health centers, to support system-wide planning. In response to user feedback, IDS has developed time-saving reports and dashboards focusing on health system priorities, such as Quality-Based Procedures, health equity, and OHT indicator monitoring. The platform is piloting data integration from Community Support Service Agencies and Hospital Ambulatory Care Clinics, with plans to capture large volumes of outpatient and community activity data. To assist smaller partners without analytical capacity, IDS has developed a new Agent Log-in process, enabling organizations to act on behalf of others in the IDS environment, particularly benefiting OHT partners.
 Labour Relations
Labour Relations
In a series of significant labor relations developments, negotiations for 2024 renewal collective agreements were concluded with CUPE, SEIU, and Unifor, involving interest arbitration for CUPE and SEIU. The 2023 renewal collective agreement with PARO was finalized in September, while preparations for ONA collective bargaining, slated for early 2025, have commenced. Additionally, reopener negotiations with PIPSC regarding Bill 124 were concluded, including interest arbitration, and the 2024 renewal collective agreement with OPAA was settled in June. Ongoing efforts continue with OPSEU Central Pay Equity Maintenance, a project without a specific end date.
This work is complemented by the quarterly publication of a Labour Relations Bulletin, highlighting major arbitration decisions.
Enhancing Hospital Capacity for Research and Clinical Care
In March 2024, the Hospital Research and Innovation Committee (RIC) initiated the development of a Community of Practice (CoP) to enhance research coordination across hospitals. The pilot CoP launched in September 2024 with seven community hospitals collaborating to define objectives and create a workplan. As of October 2024, efforts were underway to recruit seven to eight academic hospitals to join the pilot, with the aim of sharing research resources and co-designing a Teams-based platform for the CoP.
Concurrently, the RIC Integration Working Group addressed barriers to integrating research and clinical care. Following a jurisdictional scan in 2023, the group identified funding challenges as a major obstacle in May 2024. To overcome this, they proposed enhancing coordination across funding mechanisms, increasing engagement with the Ministry of Colleges and Universities, and developing a branding strategy for hospital-based research innovation in the province.
Building Internal Capacity to Support Hospitals
To lead upcoming work in support of our hospitals, the OHA appointed a Chief, Innovation and Transformation Officer (CITO), tasked with improving hospital funding methodology to drive innovation and integration across health services. The OHA's focus for the coming year includes two major areas of innovation: health care delivery innovation, which implements new solutions leveraging technologies for commercial and societal impact, and health system innovation, which explores innovative ways of planning, funding, and coordinating health services to enhance patient outcomes and population health.
In addition, the OHA created a new functional area dedicated to exploring and iterating crucial policy and research questions. By combining long-term health policy with applied research and establishing clear objectives, the OHA strives to ensure that its resources remain relevant and applicable for hospitals and policy makers, ultimately creating value through unique solutions with real-world impact.
In support of streamlining the overall startup time for clinical trials, the OHA participated in Clinical Trials Ontario's Model Clinical Trials Agreement Committee. This initiative aimed to create a universal agreement template to expedite clinical trial start-up times in Ontario. The final version of the Universal Agreement for Clinical Trials (UACT) template was announced in early November 2024 and shared with OHA member hospitals.
Looking Forward
Through 2025, we remain committed to supporting hospitals with present-day challenges while also empowering them to drive necessary systemic changes. Our focus on immediate support and future-oriented transformation underscores our commitment to ensuring a robust and responsive health care system for all Ontarians.
Our commitment to Ontario's hospitals and the health of all Ontarians remains unwavering as we navigate the challenges and opportunities that lie ahead.