Helen Lampi, (Top L), Director of Nursing at Castleview Wychwood Towers, welcomes back members of UHN's Mobile Team Vaccine - flashing "V" for vaccine - last week as they prepare to administer second doses of Moderna's COVID-19 vaccine. On December 31, the team kicked off the vaccination drive at the home. (Photo: Brian Hodges)
It has been a long and difficult pandemic year – especially for those working in Ontario's health care system. A bright spot in early 2021 was watching as the first round of COVID-19 vaccines rolled out to residents of long-term care and high-risk retirement homes. The health care workers leading the charge in hot spot regions documented their success on social media using #TeamVaccine.
Celebrating this progress gives us the hope and energy we need to continue the hard work– and it's an opportunity to learn valuable lessons as we prepare to expand the vaccination effort more broadly. The Association of Family Health Teams of Ontario, the Ontario College of Family Physicians and the Ontario Hospital Association spoke to some of these experts to hear their stories. One common theme was very clear: collaboration between stakeholders from different parts of the health care system has been the most important ingredient to getting as many vaccines in arms as quickly as possible.
Activating Pre-Existing Relationships
It took only 24 hours between when the first shipments were delivered to the University Health Network (UHN) and when long-term care resident Doreen Bible became the first Ontarian to receive the Moderna vaccine. Dr. Brian Hodges, UHN's Executive Vice President Education & Chief Medical Officer, says the high-speed effort was a bit like "building the airplane while you're flying it." Thankfully, UHN was able to call on the ready-built structure of the Family Health Team at Toronto Western Hospital – who were experienced working as a team, and ready to help.
The organizational capacity of hospitals plus skilled primary care practitioners became a combination that would power efforts across Toronto, spreading to engage teams from nine hospitals to vaccinate about 160 long-term care homes, retirement homes and other congregate living settings. Family physician Dr. Tia Pham describes how members of the East Toronto Family Practice Network were eager to help Michael Garron Hospital get needles into arms. "The hospital took care of all the logistics, and we all jumped in and helped with physician staffing, alongside hospital nurses," she says.
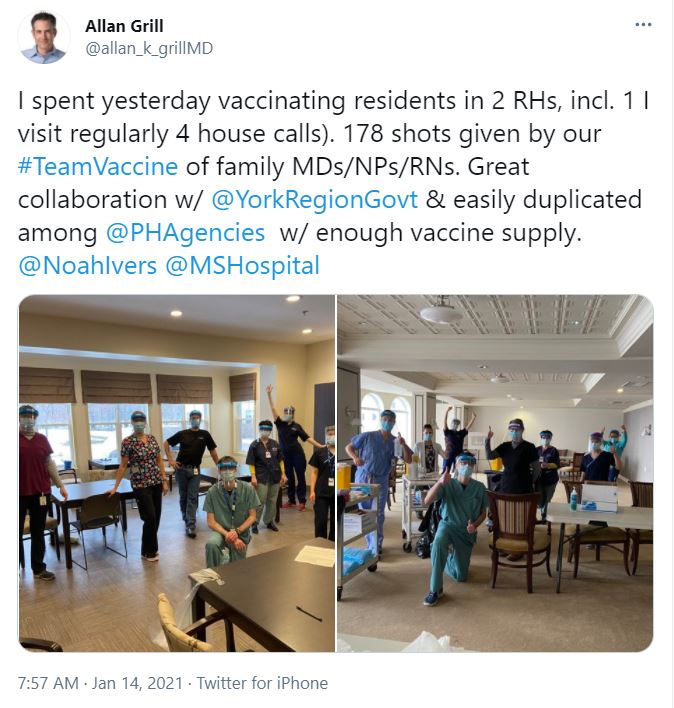 Meanwhile in York Region, Dr. Allan Grill, Chief of Family Medicine at Markham Stouffville Hospital, describes the initial outreach from the Markham Family Health Team, where he is also Lead Physician, to York Region Public Health. When public health put out the call for additional volunteers so they could vaccinate long-term care and retirement homes more quickly, he says "we overwhelmed them with enthusiasm." Within 24 hours, they had the names of 125 family physicians and interprofessional health care providers ready to help.
Meanwhile in York Region, Dr. Allan Grill, Chief of Family Medicine at Markham Stouffville Hospital, describes the initial outreach from the Markham Family Health Team, where he is also Lead Physician, to York Region Public Health. When public health put out the call for additional volunteers so they could vaccinate long-term care and retirement homes more quickly, he says "we overwhelmed them with enthusiasm." Within 24 hours, they had the names of 125 family physicians and interprofessional health care providers ready to help.
All the experts agreed that leveraging pre-existing relationships and effective communication helped each of the partners involved in the vaccination effort play to their strengths, whether they came from acute care, primary care, public health, or the long-term care and retirement homes themselves.
(Pictured on the left, Tweet from Dr. Allan Grill)
Stepping Outside of Siloes and Comfort Zones
In an effort where speed could literally save lives, a willingness to step outside of their siloes of the health care system was essential. "Primary care is an important partner to the acute care sector and public health sector in getting everyone vaccinated as fast as possible," says Dr. Pham. "We just have to get rid of all our sector definitions and get the job done, together, all-hands-on-deck."
This flexible and nimble approach started when interdisciplinary teams of hospital IPAC specialists and family physicians supported homes dealing with outbreaks earlier in the pandemic, and naturally extended into the vaccination effort, with relationships getting stronger along the way. Each of the experts we spoke to had examples of this principle in action – from different hospitals vaccinating homes in one another's neighborhoods to long-term care staff preparing for and supporting vaccination events.
The vaccination effort required personal flexibility too. Chantal Simms, a social worker who is part of the Women's College Hospital Academic Family Health Team, was redeployed from her usual role providing virtual mental health psychotherapy to acting as a site lead supporting vaccination efforts. The work has meant moving outside of her comfort zone, but she says it has been very rewarding to "feel the energy and like you are part of something really incredible."
One of Dr. Hodges' favourite parts of joining the long-term care vaccination teams has been seeing the apprenticeship model in action. As a psychiatrist, he was able to share his expertise with his team to help residents with dementia or behavioural challenges remain calm. In exchange, he was trained by a nurse on how to draw precious vaccine doses from the vial without waste. It's a model that makes the best possible use of the team's collective strengths and experience.
Integrated Care in Action
The overall vaccination effort is just getting started, and as supply stabilizes and the pace increases, everyone agrees that teamwork will continue to play an important role. Hospitals, primary care and public health are already working together to examine options that make the best use of the health system's existing resources and skills. Completing the largest vaccination campaign in the province's history is a daunting task, but good news stories like #TeamVaccine prove it can be done because everyone pulls together.
Dr. Hodges points out that this experience has potential well beyond vaccines. "What we're doing is trying to knit together the health care system in a way that's more adaptive and responsive for what people need," he says. He has already started conversations around future opportunities to collaborate with long-term care homes post-pandemic.
The experts hope that relationships formed and strengthened to respond to COVID-19 will last long beyond the pandemic and contribute to building a better-integrated health system in general. Such relationships are a prerequisite to Ontario Health Teams and other models that put patients at the centre and focus on what's best for them. For example, Dr. Pham hopes that more hospitals will be inspired to welcome closer relationships with primary care partners.
"One of the things that I hope will happen after this pandemic is over," says Dr. Grill, "is to look at how hospitals, primary care, Ontario Health Teams and public health came together and the power we have in partnership. Let's leverage what's happening now to continue these relationships going forward. That's what's really going to strengthen the health system in Ontario."
Read more about #TeamVaccine from UHN.