COVID-19 has exposed many existing gaps in Ontario's health system, including inequitable health outc omes for different sociodemographic populations. To explore this important issue, the OHA looked at evidence of a potential relationship between segmentation by racial community and select hospital-related, COVID-19 indicators. Given the limited collection and availability of individual-level race information, the OHA worked with Integrated Decision Support (IDS) Business Intelligence Solution to apply the 2016 Ontario Marginalization Index (ON-MARG) to see how the ethnic concentration of a patient's community may be linked to health outcomes.
omes for different sociodemographic populations. To explore this important issue, the OHA looked at evidence of a potential relationship between segmentation by racial community and select hospital-related, COVID-19 indicators. Given the limited collection and availability of individual-level race information, the OHA worked with Integrated Decision Support (IDS) Business Intelligence Solution to apply the 2016 Ontario Marginalization Index (ON-MARG) to see how the ethnic concentration of a patient's community may be linked to health outcomes.
IDS is a healthcare analytics platform that hosts a rich dataset from many health service providers (HSPs) in Ontario, which are typically submitted to IDS 30-60 days post encounter. Within IDS, coded hospital data is available for the initial wave of the pandemic, allowing for early and widespread analyses of COVID-19 that can support decision making for subsequent waves of the pandemic. While many different COVID-19 health factors and outcomes can be examined using IDS data, such as the rate of hospitalization, occurrence of existing chronic conditions, ICU usage, ventilation rates, mortality rates, etc., this analysis focuses only on the rate of COVID-19 emergency department (ED) visits per population.
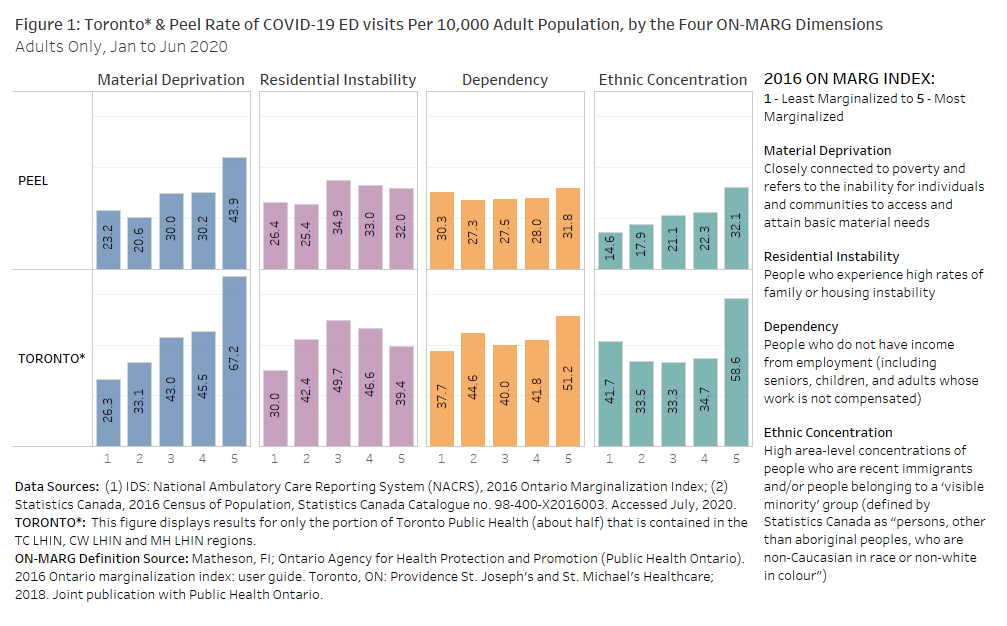
In Figure 1, patients were assigned a marginalization score based on the neighbourhood (specifically dissemination areas of 400-700 people) in which they lived. These results highlight the rate of COVID-19 ED visits for residents of Peel Public Health Unit and the portions of the Toronto Public Health Unit currently available in IDS (hospitals in the north east portion of the Toronto Public Health Unit are not yet part of IDS) because Toronto and Peel have high rates of COVID-19 ED visits and have the largest concentration of ethnically diverse populations within IDS Patient Regions. Charts of other IDS regions, as well as full references and methodology are provided in the attached detailed report.
The analysis shows that in Peel region, there was a clear increasing trend in the rate of COVID-19 ED visits as the ethnic concentration of the patient's neighborhood increased. A less clear incremental trend with respect to ethnicity is visible in Toronto, but it is worth noting that those living in the most ethnically diverse neighborhoods (quintile 5) have a considerably higher rate than those in all other quintiles. While not the primary focus here, a look at the other ON-MARG dimensions reveals that in both these regions, COVID-19 ED visits increased as the material deprivation (and to a lesser extent dependency) of the patient's neighborhood increased.
To see if this connection between higher rates of COVID-19 ED visits and the ethnic concentration of a patient's neighbourhood persists or is pronounced at a more localized level, the next figures display Toronto and Peel regions subdivided into LHIN Subregion areas.
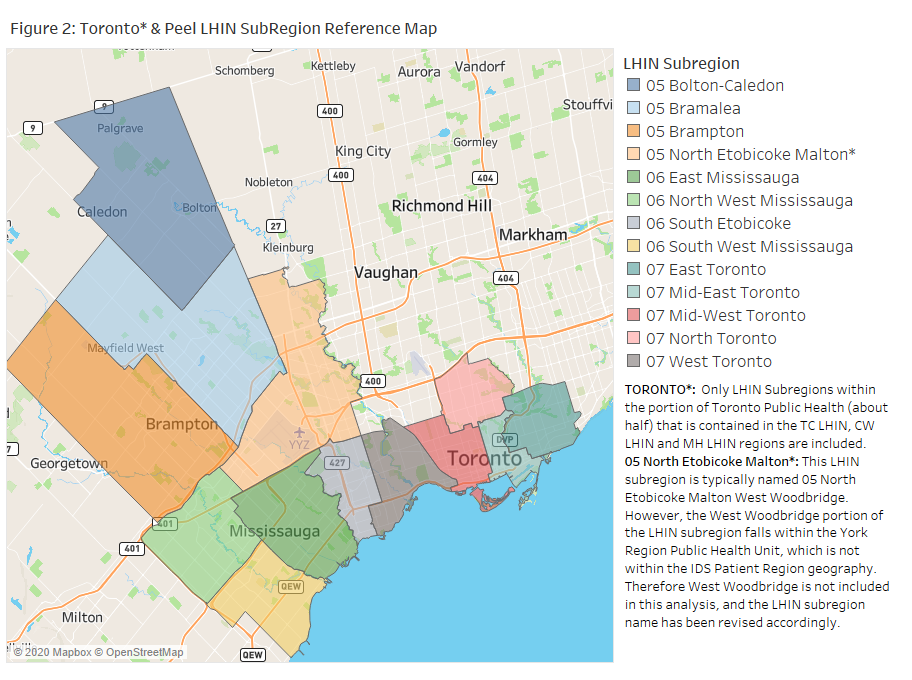
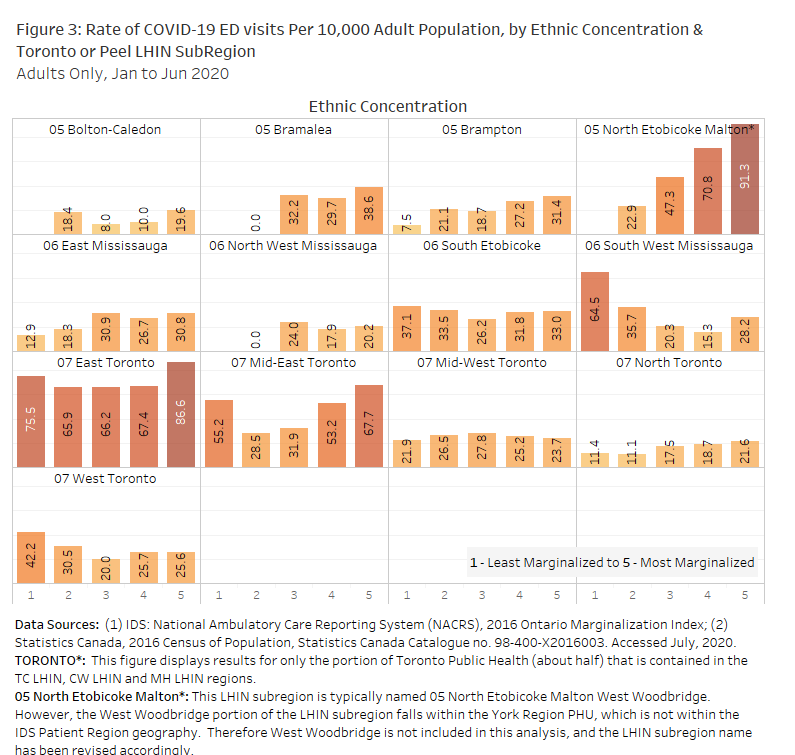
Figure 3 shows that within certain LHIN Subregions, such as Brampton, North Etobicoke Malton, East Mississauga, and North Toronto, there is an increasing trend in the rate of COVID-19 ED visits per population as the ethnic concentration of the patient's neighbourhood increases. Interestingly, in other sub-regions such as West Toronto and South West Mississauga, the rate of COVID-19 ED visits per population decreases with ethnic concentration.
While only a proxy for analysis using individual-race data, the ON-MARG ethnic concentration dimension reveals that, in at least some areas of the province, neighbourhoods with higher ethnic concentration are more likely to see COVID-19 ED-related visits. This supports recent studies that have revealed disproportionate incidence of COVID-19 as evidence of race-based inequities in health outcomes. This demands further examination as to its root causes and the development of appropriate responses to close these health care gaps.
Additional tables, as well as more detailed methodology and references, can be found here.
About the Authors
Michelle deJonge is an IDS Performance Advisor at Hamilton Health Sciences and IDS' resident epidemiologist (dejongem@hhsc.ca).
Anthony Jonker is the Chief, Data and Analytics at the Ontario Hospital Association (ajonker@oha.com).
About IDS
The Integrated Decision Support (IDS) business intelligence solution is a healthcare analytics platform designed to support planning, system improvement and performance monitoring, outcome measurement and population health equity. Created 11 years ago as a partnership of organizations wishing to share data to enable improved measurement and outcomes, IDS includes a multi-organization (80+) unified data architecture for a longitudinal patient journey, hosted and delivered by Hamilton Health Sciences. IDS includes data from half of Ontario's hospitals, as well as home and community care data, and data from select primary care, community health centres, and EMS locations. IDS is governed by providers, for providers and continues to grow. In partnership with the OHA, IDS is steadily increasing the number of organizations in its network as it works toward a vision to enable powerful integrated analytics and planning for health providers across all of Ontario.
For more information about whether your organization already has access to IDS or to find out how to join, please contact Wendy Gerrie, Director Regional Decision Support and IDS Lead at gerriew@hhsc.ca.