Humber River Health (Humber) has recently revitalized its Chemical Dependency Program (CDP), aimed at refining and expanding its services support for individuals struggling with substance use concerns. This redesigned program signifies a broader shift towards a more integrated and comprehensive approach to addiction care, and reflects Humber's commitment to addressing the complex needs of its patients.
The CDP at Humber is an inclusive service designed to address various substance use concerns. It offers a range of treatments, including group therapy, individual counseling, and education sessions for individuals. The program provides thorough assessments, medication recommendations, and psychiatric consultations if required, addressing both substance dependency and concurrent mental health disorders. It supports a spectrum of care goals, from abstinence to harm reduction, and has adapted its model to better meet the needs of patients within the Hospital and Emergency Department (ED).
Originally focused on alcohol use disorders, the CDP now addresses various types of substance use with a diverse array of medications. The program is supported by a multidisciplinary team, including psychiatrists, nurse practitioners, registered nurses, social workers, addiction counselors, and other specialists tailored to patient needs. Over the years, the CDP has continually evolved to enhance its offerings and adapt to changing healthcare demands.
Strategic Redesign and Implementation
Originally stationed at the legacy Keele Street site with limited integration into Humber's main services, the program's relocation to the Wilson site marked the start of a pivotal shift to support the patients who are within the building. However, with this move, it became clear that the programs and services needed to be updated, as the acuity and complexity of the patient population changed, and barriers were present between the Hospital and community.
“The impetus for the redesign was to enhance the accessibility and quality of care for our patients, as well as individuals who are frequently visiting the ED due to lack of access to care," says Darlene Ginsberg, the Manager of Adult Mental Health and Addictions Outpatient Programs at Humber. “Additionally, we want to support individuals who are coming in with very acute clinical presentations, which were not the services that we had designed previously within the Chemical Dependency Program."
The redesign, which concluded its initial stage in February 2024, implemented the following elements:
- A Knowledge Hub within Humber's internal portal to centralize information and resources, thereby facilitating smoother day-to-day operations for clinicians and enhancing the overall provider experience.
- The provision of Naloxone kits, which are emergency kits used to manage potential opiate overdose. This proactive step ensures patients and their loved ones are equipped with the necessary tools to respond to potential overdose situations. Although available at various pharmacies, Humber's workflow enable the kits to be distributed to patients during discharge.
- The update of Meditech order sets for managing withdrawal associated with alcohol and opioid use disorders, enabling patients to receive treatment in a standardized way.
- The introduction of Sublocade as a treatment option. This long-acting, monthly injectable medication allows for more regular dosing, and is more convenient for patients.
- A newly developed brochure, co-designed with Ontario Health Team's (OHT) substance use partner agencies, which provides a wide range of resources and information for patients and their families.
- Launched a guideline for tools and methodologies for standardized assessments.
Quantitative Results
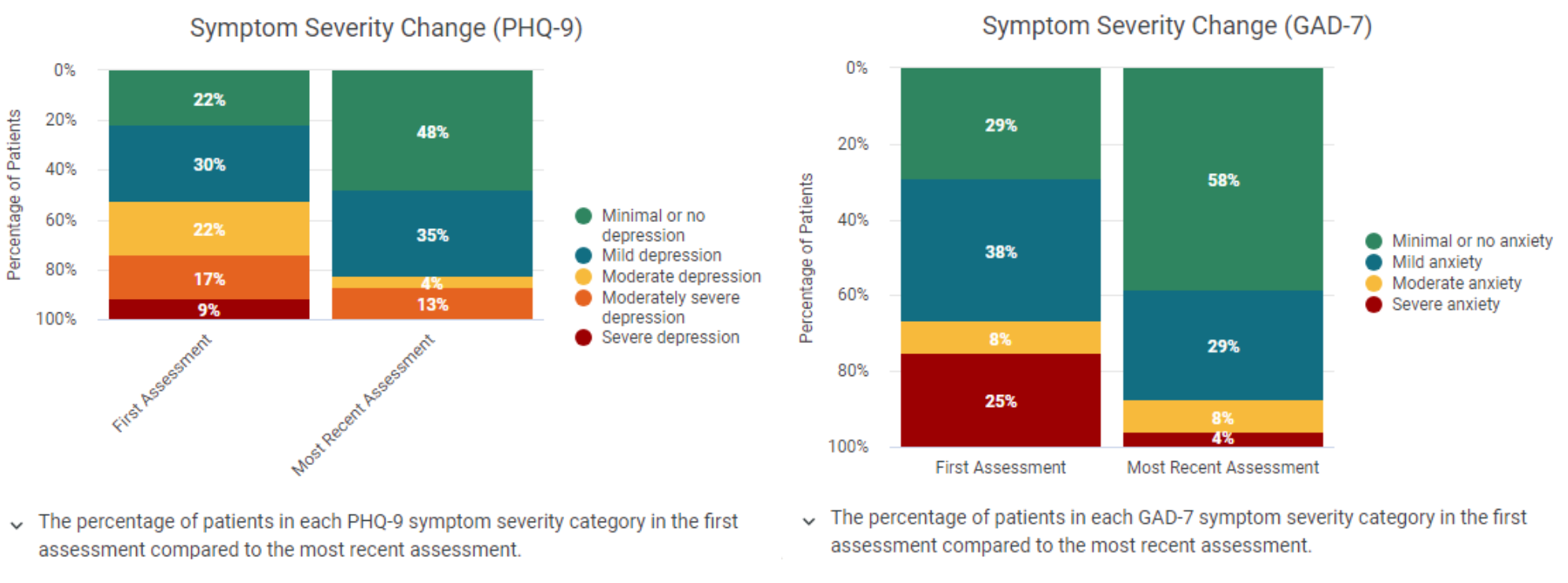
The redesigned CDP at Humber has yielded promising early results, particularly in the areas of mental health outcomes for patients. Utilizing the PHQ-9 and GAD-7 scales, which measure depression and anxiety respectively, the program tracked the progress of 44 patients from their initial assessment in early December to their most recent assessment at the end of March. The data reveals a positive shift in mental health states over this short period of time. Specifically, the depression scores improved; at the start of treatment, only 22 per cent of patients showed minimal or no signs of depression, but by the end of the treatment period, this figure had more than doubled to 48 per cent. Notably, there were no patients remaining in the "severe depression" category by the end of their treatment.
Similarly, anxiety scores saw even more substantial improvements. The percentage of patients categorized with severe anxiety plummeted from 25 per cent at the beginning of treatment to just 4 per cent by the most recent assessment. Moreover, the majority of patients were found to be in the “minimal or no anxiety" category at the conclusion of their treatment period.
Looking Ahead
This multifaceted approach allows the CDP to cater to a diverse range of substance use concerns, from opioid and alcohol dependency to concurrent mental health issues, with a range of treatment options including medication recommendations, opiate agonist therapy, anti-craving medications, group therapy, as well as education and counselling. The results of the program's redesign, although in the early stages, are already promising. This success is further exemplified by the positive feedback received from the PHQ-9 and GAD-7 results.
Humber is actively addressing the high volume of ED visits by developing strategies to streamline the transition from ED care to outpatient services. The hospital has initiated a pilot process to enhance this linkage, from which valuable lessons have already been learned, and improvements continue to be made. Looking ahead, Humber plans to work with their ED and community partners to examine referral processes with an aim to further enhance access to care. They are also working on expanding services to better meet the needs of patients who are in the pre-contemplative stage of change.
Humber's revamped Chemical Dependency Program embodies a forward-thinking approach to chemical dependency treatment. “By integrating a range of support services, standardizing care protocols, and prioritizing patient and family engagement, Humber is setting a new standard in addiction treatment," says Darlene. “The program's ongoing evolution, driven by a dedication to patient empowerment and innovation, sets a precedent for the future of addiction services, promising a brighter, healthier future for patients and their families."