What is alternate level of care?
The Ottawa Hospital (TOH), like other hospitals across the province, has seen a dramatic rise in patients designated Alternate Level of Care (ALC).
An ALC patient is someone who is currently occupying a hospital bed but no longer needs the intensity of resources/services provided in this setting. For our hospital, these patients may have completed their acute phase of treatment, are ready for discharge, and now need different kinds of care, such as rehabilitation, long-term care, or home care.
Hospitals are designed to provide acute care and staying longer than necessary can lead to poorer outcomes and experiences for these patients and their loved ones.
To better address the challenges of ALC patients, it's vital that hospital data reporting is accurate.
In the past, the terms ALC and medically inactive were used interchangeably. Medically inactive patients (whose care is less acute) were then included in TOH's total ALC count. However, 20 – 25 per cent of patients did not fully meet the province's ALC definition.
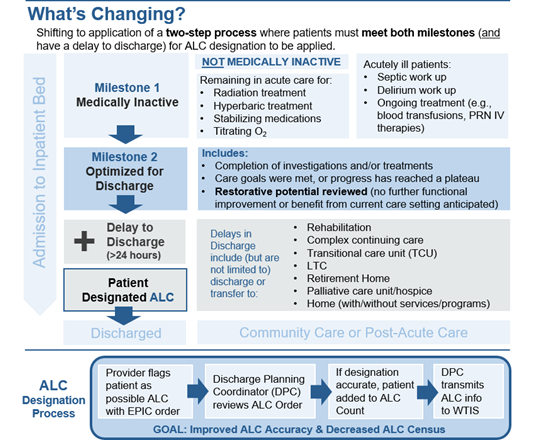
To avoid inflated ALC counts, TOH developed workflow changes in EPIC to ensure that patients were only designated ALC when they met certain criteria. A secondary process was also developed to help physicians designate patients as medically inactive.
Instead of writing an ALC order, physicians now flag patients as medically inactive when acuity diminishes and request a review for ALC eligibility. A Discharge Planning Coordinator then reviews each medically inactive order to determine alignment with the ALC definition.
By ensuring alignment with the province's ALC definition, this workflow allows for more accurate reporting – a key step aimed at addressing further ALC challenges.
Under TOH's new workflow, patients are only designated ALC when they meet these milestones:
- Medically inactive
- Optimization for discharge is complete
- Restorative potential has been reviewed
- Delay in discharge of greater than 24 hours
Medically inactive orders are reviewed regularly, and patients are transitioned to ALC status once they meet all the milestones. Only then are they recorded as ALC in our EMR, EPIC, and the provincial Wait Time Information System.
Below is an educational tool outlining the workflow change process and ALC designation.
Since January 2024, TOH has decreased ALC volumes by more than 10 per cent.
“Ensuring that the right patients are designated as ALC is crucial for many reasons. With more accurate reporting, we can better understand our ALC population and how to support them through the hospital system and towards discharge. This optimizes hospital space and improves flow for patients needing urgent and intensive treatment,“ said Carol Murphy, Program Director of Regional Subacute Coordinated Access & ALC Strategy at The Ottawa Hospital. “This allows patients to receive the right level of care in the right setting, which is essential for their recovery and overall well-being."
With the workflow changes, TOH has surpassed the reduced ALC target set by Ontario Health. Clarifying the definition has ensured that ALC volumes are more accurately represented – marking a positive step towards addressing ALC challenges within the health care system.